Would you trust AI to write your prescription?
Plus: My conversation with Reed Jobs
I’m heading to the Economist AI in Health Summit this week. If you’re around, find me and say hi!
Speaking of AI in health, I know it’s a topic on all of our minds. The podcast episodes we do on AI get the most listens. We’ve had the founders of Abridge, Ambience, Commure on this year— and have a few more very exciting episodes coming up.
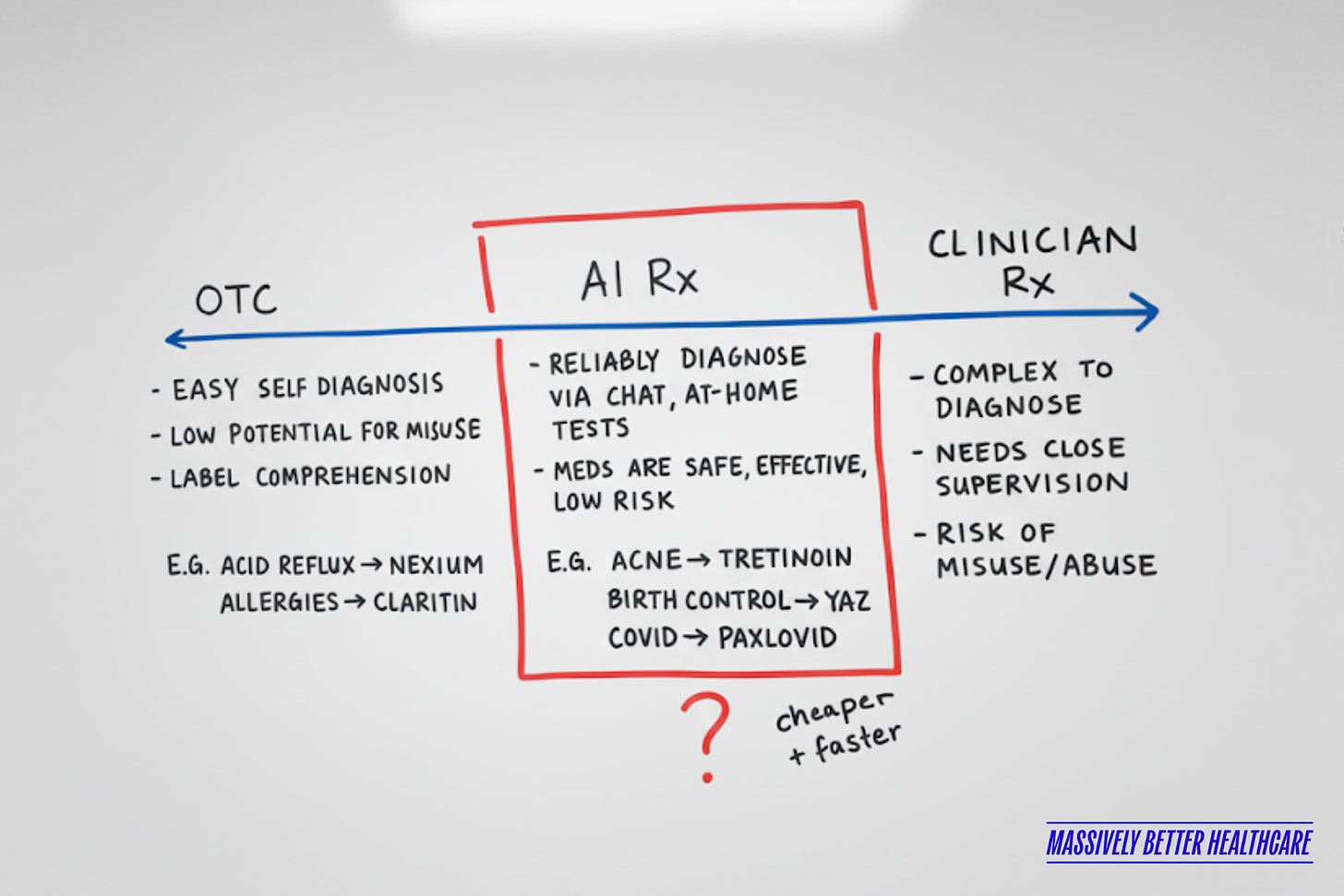
When it comes to “AI doctors,” we hear a lot of extremes: either AI will replace doctors entirely, or it won’t (and shouldn’t) replace any part of their role outside of administration. The reality, of course, is somewhere in between.
Here’s how I’ve been thinking about it:
Today, there are only two paths to prescription treatment in the U.S.:
1️⃣ Over-the-counter (OTC): Conditions you can easily self-diagnose and manage. Think allergies → loratadine (Claritin), heartburn → famotidine (Pepcid).
2️⃣ Prescription-only: Conditions where you need to see a clinician for a diagnosis and prescription.
Over time, some drugs have appropriately moved from the second bucket to the first as regulators determined they were safe enough for self-diagnosis and self-management. Allegra, Nexium, Zyrtec, Narcan were once prescription-only. (Here’s the full Prescription to Nonprescription Switch List).
Arguably, there should be a third bucket in between these two, where validated, licensed AI models can safely handle the “low-hanging fruit” from the prescription-only bucket. For conditions that are:
Objective and reliably diagnosable via data, symptoms, or at-home tests
Treated with medications that are safe and effective, with a low risk of misuse
Currently overloading our healthcare system, but don’t truly need a human doctor’s time for every case
I’m a visual person, so I mapped it out here:
Just as we have a formal process for the Rx-to-OTC switch, we could imagine a similar process for establishing a Rx-to-AI category.
To me, this feels like a feasible near-term future. We are at an inflection point in healthcare:
Demand is there. Patients already want—and are getting—prescriptions asynchronously without ever seeing a clinician. Just look at Hims, Ro, Sesame, etc.
The work itself is ripe for automation. On these platforms, clinicians are doing highly repetitive, checklist-driven reviews of online questionnaires. It’s important work (because it’s legally required), but not the best use of scarce medical expertise. AI, when validated and licensed, could perform this task just as safely and consistently.
Technology is ready. We already have FDA-cleared AI tools that read medical images, triage symptoms, and support diagnoses. The idea that AI could review structured questionnaires or simple lab results is well within today’s capabilities.
Layer on the realities of a clinician shortage and spiraling healthcare costs, and the case for an AI-to-Rx category becomes even stronger.
So what would it take?
✅ Regulation. These tools would need to be able to prescribe legally. Regulators would need to decide which tools are approved for this purpose and for which drugs.
✅ Trust. Patients will need to believe an AI is just as safe—and just as accountable—as a human clinician.
✅ Supervision. Patients must always have a clear path to escalate to a human clinician if their case is more complex than it appears.
I actually think primary care practices would be the best place for this to start. They’re already the front door to the healthcare system, already under tremendous pressure, and already built on triage. Embedding AI prescribing into primary care could help practices handle routine, low-risk cases more efficiently—while freeing clinicians to focus on patients who truly need their expertise.
This feels like a future worth building. Would love to hear your thoughts in the comments!
🎧 New Podcast Episode with Reed Jobs & Matt Bettonville of Yosemite
After losing his father, Reed Jobs committed himself to making this the last generation that loses parents to the disease.
Reed now leads Yosemite, a venture fund spun out of Emerson Collective in 2023, alongside Investor Matt Bettonville. Yosemite pairs life sciences and digital health investments with a grantmaking model to accelerate cancer research and ensure breakthroughs actually reach patients.
In this episode, we cover:
📉 The tension between drug pricing, patient access, and real-world value
🩺 Digital interventions that have outperformed cancer drugs in survival outcomes
🧪 Why phase 3 clinical trials are so costly, and how synthetic control arms could change that
🧬 The promise and limits of early detection—from liquid biopsies to at-home pap smears
🌍 The global race for healthcare innovation and why the U.S. can’t afford to fall behind
Listen now on Apple, Spotify, or wherever you listen to podcasts.
How you can support my work:
⭐️ Leave a review for the Heart of Healthcare podcast. It takes just five seconds!
💻 Download a copy of my digital health startup database.
🫶 Share this email with a digital health friend.
💸 Become a paid subscriber or sponsor!



I immediately went to thinking of Strep throat and antibiotics. I do think this is something that many patients could get on board with when they know a likely outcome.
Interesting idea Halle. This has merit. I can see this starting with physician oversight where a patient questionnaire is largely reviewed by AI but any responses that don’t fit the framework get kicked to a physician for review. Telehealth on the backend would be critical for further evaluation of select patients when needed. This would likely result in 5-10% of patients needing a consult.